Save Time in the Toilet and Avoid Embarrassing Moments!
Do any of these situations sound familiar?
- Rushing to the toilet during a meeting or while shopping?
- Straining for what feels like forever in the bathroom?
- Feeling anxious about frequent flatulence in public places like elevators, cinemas, or trains?
- Constant bloating that makes your belly look like you’re expecting (when you’re definitely not)?
You’re not alone—and you’re not without options.
Let’s be clear—this isn’t an embarrassing topic. Constipation, diarrhoea, bloating, and flatulence are common gastrointestinal (GI) issues that affect people across the country, about 1 in 10 Malaysians.
Today, we’re focusing on constipation and diarrhoea. While they may seem like complete opposites, they can actually occur together or affect the same person at different times. Both conditions can seriously impact your daily activities and quality of life, leading to discomfort, pain, and even anxiety.
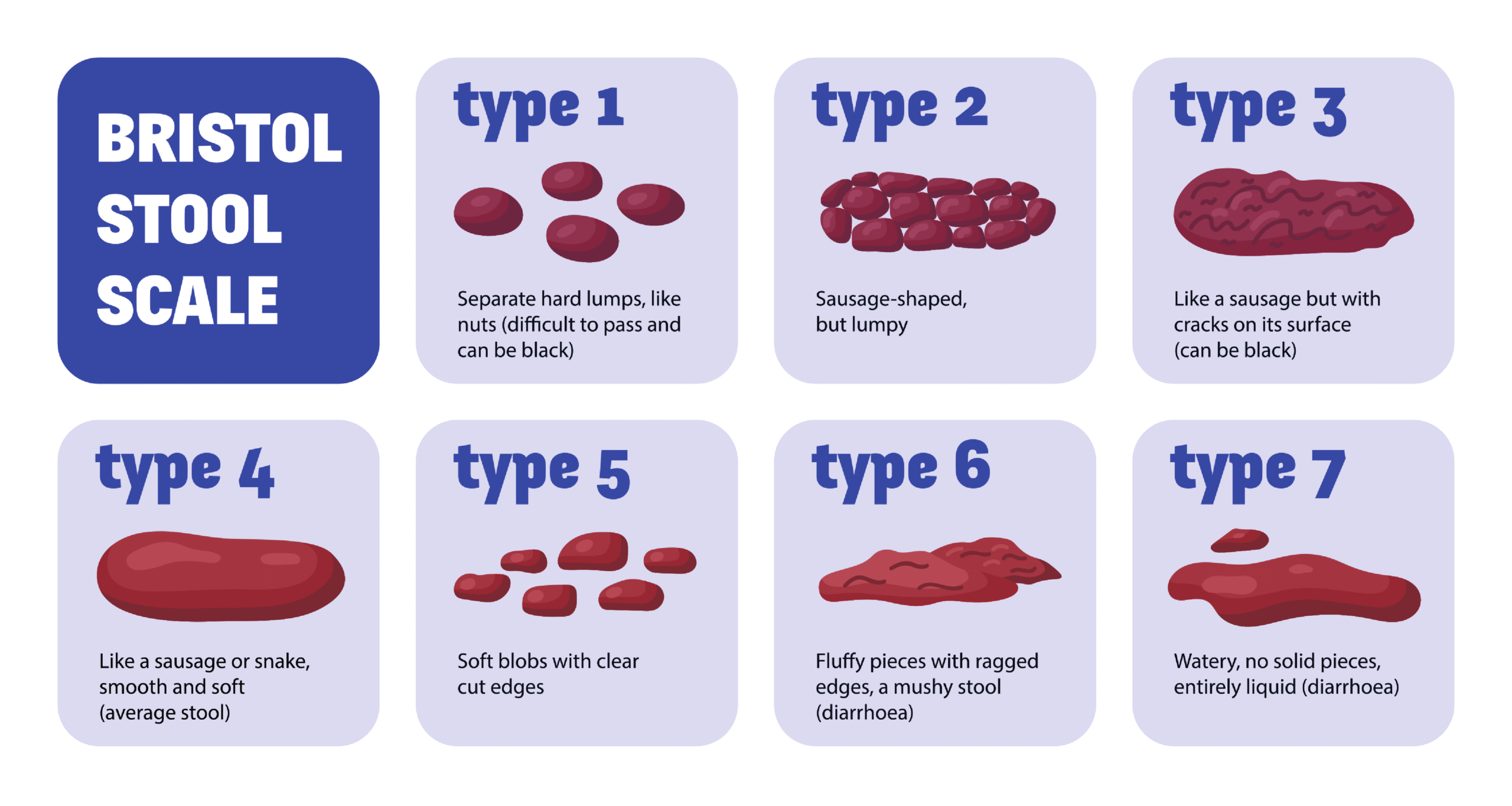
Constipation is characterized by infrequent bowel movements, typically occurring fewer than three times per week, and is often accompanied by difficulty passing stools. Symptoms may include straining during bowel movements, hard or lumpy stools, a sensation of incomplete evacuation, and abdominal pain or bloating.
Various factors can contribute to constipation. A diet high in processed foods and sugar but low in fiber can lead to digestive problems and inflammation. Inadequate fluid intake can also cause stools to become hard and difficult to pass. Physical inactivity or a sedentary lifestyle can reduce bowel motility (the movement of food through the digestive tract), resulting in constipation.
Certain medications, such as opioids, antacids containing aluminium, antidepressants, and iron supplements, as well as medical conditions like diabetes and hypothyroidism, can adversely affect bowel function and contribute to constipation.
Additionally, stress and reduced intestinal mucus production may indirectly contribute to constipation. Women and the elderly, especially those with lower muscle mass and metabolic rates, are more prone to this condition.
On the other hand, diarrhoea is characterised by the frequent passage of loose or watery stools and can be either acute or chronic. Symptoms include increased stool frequency (more than three times per day), watery consistency, abdominal cramps, and an urgent need for bowel movements.
Diarrhoea can result from various causes, including infections caused by bacteria, viruses, or parasites, as well as food intolerances or malabsorption issues (such as sensitivities to lactose, fructose, fat, or gluten). Additionally, stress, allergic reactions to certain antibiotics that disrupt gut bacteria, and conditions such as IBD (Inflammatory Bowel Disease) or IBS (Irritable Bowel Syndrome) may also lead to diarrhoea.
If you are experiencing ongoing diarrhoea, constipation, or both—especially when accompanied by abdominal pain and cramps—it may indicate IBS. In contrast, if your diarrhoea is persistent and accompanied by abdominal pain, cramping, fatigue, and loss of appetite, it may be associated with IBD. In such cases, it is advisable to undergo a thorough medical evaluation.
There are two main types of IBD: Crohn’s disease and ulcerative colitis. The exact causes of both IBD and IBS are not fully understood, but they are believed to result from a combination of genetic and environmental factors.
In recent years, the consumption of live bacteria, or probiotics, has become a popular approach for relieving gastrointestinal problems. While probiotics are sometimes prescribed by doctors, many people still do not fully understand what they are or how they work. To grasp their role, it’s important to understand the ecosystem within our digestive tract, known as the gut microbiota.
The gut microbiota, or microbiome, is essential for maintaining digestive health and supporting the immune system. It consists of trillions of microorganisms—including bacteria, fungi, and viruses—that inhabit the gastrointestinal (GI) tract. A balanced gut microbiota (a healthy ratio of beneficial to harmful bacteria) is crucial for effective digestion, nutrient absorption, protection against pathogens and toxins, and modulation of immune responses. It can even influence our mood and behaviour.
Harmful, or pathogenic, bacteria can produce toxins and contribute to the process of putrefaction, releasing harmful byproducts such as ammonia and amines. A disruption in the gut microbiota, known as dysbiosis, or an overgrowth of harmful bacteria, can lead to digestive issues such as constipation, diarrhoea, and bloating. This is where probiotics come into play.
Probiotics are live microorganisms, often referred to as “good” or “friendly” bacteria, that provide health benefits when consumed in sufficient amounts. The two most common genera of probiotics are Bifidobacterium and Lactobacillus. These beneficial bacteria can be found in fermented foods such as yoghurt, kimchi, kombucha, and tempeh.
Probiotics help restore the natural balance of gut bacteria. Some studies have shown decreased levels of healthy bacteria in patients with Irritable Bowel Syndrome (IBS). Research indicates that specific strains of Bifidobacterium longum and Lactobacillus casei, can enhance bowel regularity by stimulating the intestinal walls and improving stool consistency, potentially alleviating constipation. Restoring normal gut flora may also reduce abnormal gas production in some constipated patients.
In managing diarrhoea, probiotics play a significant role and have been the subject of extensive research. They can help prevent infections, restore gut flora disrupted by antibiotic use, regulate immune responses, and manage chronic diarrhoea—thereby reducing symptoms and promoting overall gut health. It is believed that probiotics may decrease the adherence of pathogenic bacteria to the gastrointestinal mucosa, helping to prevent infection and inflammation.
Probiotics may also produce metabolites—compounds derived from the fermentation of dietary fiber—such as short-chain fatty acids (SCFAs), organic acids, and bacteriocins. These substances help inhibit the growth of harmful pathogens, strengthen the gut barrier, and contribute to improved digestive health. SCFAs like butyrate, propionate, and acetate serve as a primary energy source for colon cells and play a crucial role in maintaining gut integrity. Organic acids, such as lactic acid and acetic acid, create an unfavourable (acidic) environment for pathogens, while bacteriocins directly target and eliminate harmful bacteria.
Clinical studies support the effectiveness of probiotics in managing various digestive problems, including constipation and diarrhoea, in both children and adults. This underscores their value as a therapeutic option for gastrointestinal health. However, it’s important to note that probiotics are strain-specific, meaning different strains of the same species can have distinct effects. Probiotics are classified into genus, species, and strain. Each strain possesses unique characteristics and mechanisms of action. For example: Bifidobacterium (genus) longum (species) BB536 (strain).
Bifidobacterium longum BB536 is a probiotic strain discovered and developed by Morinaga, a century-old dairy manufacturer in Japan. It has been extensively studied for over 40 years and is supported by more than 200 scientific publications. BB536 has demonstrated benefits in alleviating both constipation and diarrhoea across all age groups, from infants to the elderly, and is associated with improved long-term outcomes. It has also been shown to help restore bowel frequency in elderly patients receiving enteral (tube) feeding. More recently, BB536 has been reported to be beneficial in improving symptoms of IBD and IBS.
Both constipation and diarrhoea are common gastrointestinal issues that can significantly impact daily life and overall well-being. Many individuals try to relieve constipation by drinking more water or eating more fruit, but often find little to no improvement. Similarly, those who suffer from frequent diarrhoea may attempt to eat less or avoid raw foods, but these measures are not always effective and may diminish the enjoyment of eating.
As discussed earlier, constipation and diarrhoea are often multifactorial in origin. Due to their complexity, a combination of strategies is typically more effective in managing these conditions. Probiotics offer a promising approach by helping to restore gut flora, improve bowel function, and alleviate symptoms. Therefore, incorporating probiotics alongside dietary adjustments, proper hydration, regular physical activity, and stress management can enhance digestive health.
It is advisable for individuals, especially those with pre-existing health conditions, to consult a healthcare professional to develop a personalised plan that includes the most suitable probiotic strains for their needs.
Take charge of your gut health in a holistic way. Say goodbye to awkward moments and time lost in the bathroom—welcome a smoother, more comfortable daily routine.
References
D’Souza, A. L., et al. (2016). Probiotics in the management of irritable bowel syndrome: a systematic review and meta-analysis. Journal of Gastroenterology and Hepatology, 31(3), 872-881.
Gibson, G. R., et al. (2017). The role of probiotics in the management of functional gastrointestinal symptoms: A systematic review. International Journal of Food Microbiology, 136(1), 42-54.
Hempel, S., et al. (2012). Probiotics for the prevention of antibiotic-associated diarrhoea in adults. Cochrane Database of Systematic Reviews, (11), CD006763.
Khalif, I., et al. (2009). Probiotics for the treatment of antibiotic-associated diarrhoea: a meta-analysis. American Journal of Gastroenterology, 104(4), 808-818.
Kondo, J., Xiao, JZ., Shirahata, A., Baba, M., Abe, A., Ogawa, K. & Shimoda, T. (2013). Modulatory effects of Bifidobacterium longum BB536 on defecation in elderly patients receiving enteral feeding. World Journal of Gastroenterology. 19(14): 2162-2170.
McFarland, L. V. (2010). Epidemiology, risk factors, and treatments for antibiotic-associated diarrhoea. Digestive Diseases and Sciences, 55(7), 1305-1313.
Rao, S. S. C., et al. (2015). Probiotics in the management of constipation: A systematic review. American Journal of Gastroenterology, 110(12), 1826-1930.
Rahman, M. M., Mahadeva, S., & Ghoshal, U. C. (2017). Epidemiological and clinical perspectives on irritable bowel syndrome in India, Bangladesh and Malaysia: A review. World journal of gastroenterology, 23(37), 6788–6801.
Russo, M., Giugliano, FP., Quitadamo, P., Mancusi, V., Miele, E., & Staiano, A. (2017). Efficacy of a mixture of probiotic agents as complementary therapy for chronic functional constipation in childhood. Italian Journal of Pediatrics. 43:24.
Szajewska, H., & Shamir, R. (2010). The role of probiotics in the management of acute infectious diarrhoea in children. Archives of Disease in Childhood, 95(5), 536-541.
Sung, V., et al. (2019). Probiotics for functional constipation in children. Cochrane Database of Systematic Reviews, 2019(6), CD012125.
Tamaki, H., Nakase, H., Inoue, S., Kawanami, C., Itani, T., Ohana, M., Kusaka, T., Uose, S., Hisatsune, H., Tojo, M., Noda, T., Arasawa, S., Izuta, M., Kubo, A., Ogawa, C., Matsunaka, T. & Shibatouge, M. (2016). Efficacy of probiotic treatment with Bifidobacterium longum 536 for induction of remission in active ulcerative colitis: A randomized, double-blinded, placebo-controlled multicenter trial. Digestive Endoscopy, 28: 67–74.